The Evolution and Future of Metoidioplasty Surgery
Metoidioplasty has long served as a meaningful surgical option for transgender men and nonbinary individuals seeking genital reconstruction that prioritizes erogenous sensation and erectile function. Since the first reports in the 1970s, techniques have evolved from simple clitoral release to sophisticated, single-stage procedures like the Belgrade Metoidioplasty. Today, the field is once again entering a new era, with groundbreaking innovations that promise not just refinement, but a reimagination of what this surgery can achieve.
Foundations and Early Techniques (1973–2010)
The first documented use of the clitoris in male genital reconstruction dates back to 1973, laying the groundwork for what would later become known as metoidioplasty. In the 1980s, Dr. Michael Brownstein introduced a procedure he referred to as "Genitalplasty," an umbrella term for genital reconstruction. Though never published, this early technique played a formative role, and one of Brownstein's earliest patients was Lou Sullivan, a pioneering transgender activist.
Watch an interview segment with Lou Sullivan discussing his genital surgery from 1988.
The term "Metoidioplasty" itself was coined in 1989 by Drs. Lebovic and Laub, combining Greek roots meaning "change" (meta), "male genitalia" (aidion), and "formation" (plasty). Their technique, often referred to as "Simple Meta" or "Simple Release," involved only the release of the hormonally enlarged clitoris without urethral extension or scrotoplasty.
A major advance came in 1996 when Dr. J.J. Hage published the first modern metoidioplasty technique that combined clitoral release with urethral lengthening. Using vaginal wall flaps and techniques borrowed from hypospadias repair, Hage's method allowed patients to urinate while standing and included vaginectomy and hysterectomy either before or during the procedure.
In Japan, Dr. Ako Takamatsu developed the Ring Metoidioplasty technique to address limitations in local tissue availability. This method used a labial ring flap to construct the neourethra, particularly useful in cases with narrow vaginas or underdeveloped labial tissue. While it often did not include full vaginectomy, the vaginal opening was reduced significantly.
The Belgrade Breakthrough and the Centurion Connection (2000s–2010s)
The Belgrade Metoidioplasty, sometimes called "Full Metoidioplasty," was developed in Serbia by Dr. Miroslav Djordjevic and colleagues. This highly standardized, single-stage procedure became a global benchmark. It includes clitoral lengthening through ligament release, urethral construction using oral mucosa and local flaps, complete vaginectomy, and scrotoplasty with testicular implants. Over time, refinements such as preoperative use of dihydrotestosterone gel and vacuum pumping were added to improve results.
Interestingly, it remains unclear exactly when the first Belgrade Metoidioplasty was performed, as early cases were not formally dated in the literature. Published data begins around 2009, but development may have started several years earlier.
Adding to the intrigue is the Centurion Metoidioplasty, first performed in 2002 by Dr. Peter Raphael, a Texas-based plastic surgeon—possibly predating the Belgrade method. Although never formally published in peer-reviewed literature, the Centurion technique includes all the core components of Full Metoidioplasty and introduces a distinctive refinement: the use of the round ligaments to increase girth and structural integrity of the neophallus. By mobilizing and suturing these ligaments along the shaft, the Centurion approach enhances phallic projection and helps reduce postoperative retraction, especially in patients with a prominent mons pad.
Whether these techniques were developed in parallel or whether one directly influenced the other remains uncertain.
Recent Innovations (2016-Present)
Several innovations have emerged in recent years that push the boundaries of what Metoidioplasty can offer.
In 2017, the first-ever semi-rigid erectile implant designed for Metoidioplasty patients was implanted in France. Manufactured by the Swiss company ZSI Implants, the ZSI 100 D4 prosthesis is a semi-rigid device made of silicone and silver cable that is implanted into the clitoral corpora. It’s designed to help prevent post-operative tissue contraction (loss of length), enable standing urination, and in some patients, engage in penetrative sex. Long-term data remain limited but a 2023 study by Monchablon et al. indicated potential functional benefits.
Additionally, three new techniques have emerged in the past few years that push the boundaries of what metoidioplasty can achieve: Extensive Metoidioplasty from Iran, Extended Metoidioplasty a collaboration by U.S. and Dutch teams, and Total Corporal Mobilization (TCM) from Brazil.
Dr. Shahryar Cohanzad first published details about his Extensive Metoidioplasty technique in 2016. His method builds on the Belgrade model by introducing a deeper dissection of the clitoral crura (internal erectile tissue) to increase penile length and improve erectile capacity. With Extensive Metoidioplasty, the suspensory ligaments are fully released, and the internal structures are brought forward—revealing tissue often left untouched in other versions of Metoidioplasty. Postoperative use of a traction device (Penile Enhancement Protocol) further augments length over time. In a cohort of 10 patients followed for over five years, the average neophallus length reached 8.7 cm, with 70% reporting erections rigid enough for penetrative sex. While promising, Extensive Metoidioplasty is technically demanding and associated with a higher risk of urethral complications, including fistulas and strictures. Long-term outcome data are still emerging.
Developed collaboratively by expert teams in the Netherlands and the United States, Extended Metoidioplasty first appeared in published academic literature in 2022. It prioritizes maximizing visible neophallus length and aesthetic outcomes while minimizing complications. The procedure avoids urethral lengthening by creating a perineal urethrostomy, thereby significantly reducing risks of fistulas and strictures. Scrotoplasty includes a suprapubic adipocutaneous flap to simulate testicular volume without implants. The neophallus retains preserved sensation and erectile function, although urination remains seated. This technique is particularly suited for those who wish to maintain erogenous sensation and spontaneous erections, avoid urethral complications, and achieve a natural, masculine appearance.
Total Corporal Mobilization (TCM) is a recent innovation by Dr. Ubirajara Barroso in Brazil that’s derived from reconstructive techniques used in cisgender men. Similar in concept to Extensive Metoidioplasty, it involves the complete mobilization of the internal erectile structures. In trans men, TCM repositions the internal portion of the clitoral corpora to enhance visible length and functional potential. The procedure emphasizes sensation preservation and erectile function. When combined with urethral lengthening using oral mucosa, patients may also achieve standing urination. While early outcomes are promising with low complication rates and good functional outcomes, long-term data on durability, patient satisfaction, and complication management is very limited and will be critical before widespread adoption can occur.
Watch a surgical overview by Dr. Barroso showing TCM in practice.
While both Extensive Metoidioplasty and TCM offer gains in visible phallic length and erectile function, these techniques also carry added risks due to the deep mobilization of internal erectile tissues. Dissecting and repositioning the clitoral crura involves operating near neurovascular structures that provide sensation and blood flow, increasing the potential for complications such as nerve damage, reduced erectile capacity, hematoma, or even tissue death if blood supply is compromised. Furthermore, the deep mobilization of tissues introduces risks that may impact the angle or stability of erections.
These new procedures represent technical advances as well as a shift in what patients hope to achieve. While early techniques established the foundation, newer methods like Extensive, Extended Metoidioplasty, and TCM aim to improve functional and aesthetic outcomes. The introduction of erectile implants further diversifies available choices. However, these innovations come with challenges: increased technical complexity, higher risks, and a pressing need for long-term data on safety and efficacy. As such, these approaches should be considered promising but experimental, with careful patient selection and surgical expertise being critical to successful outcomes.The evolution of Metoidioplasty over the past five decades has come from surgical creativity, patient advocacy, and evolving goals. As the field continues to expand, so too does the spectrum of options available to those seeking this deeply personal form of genital affirmation.
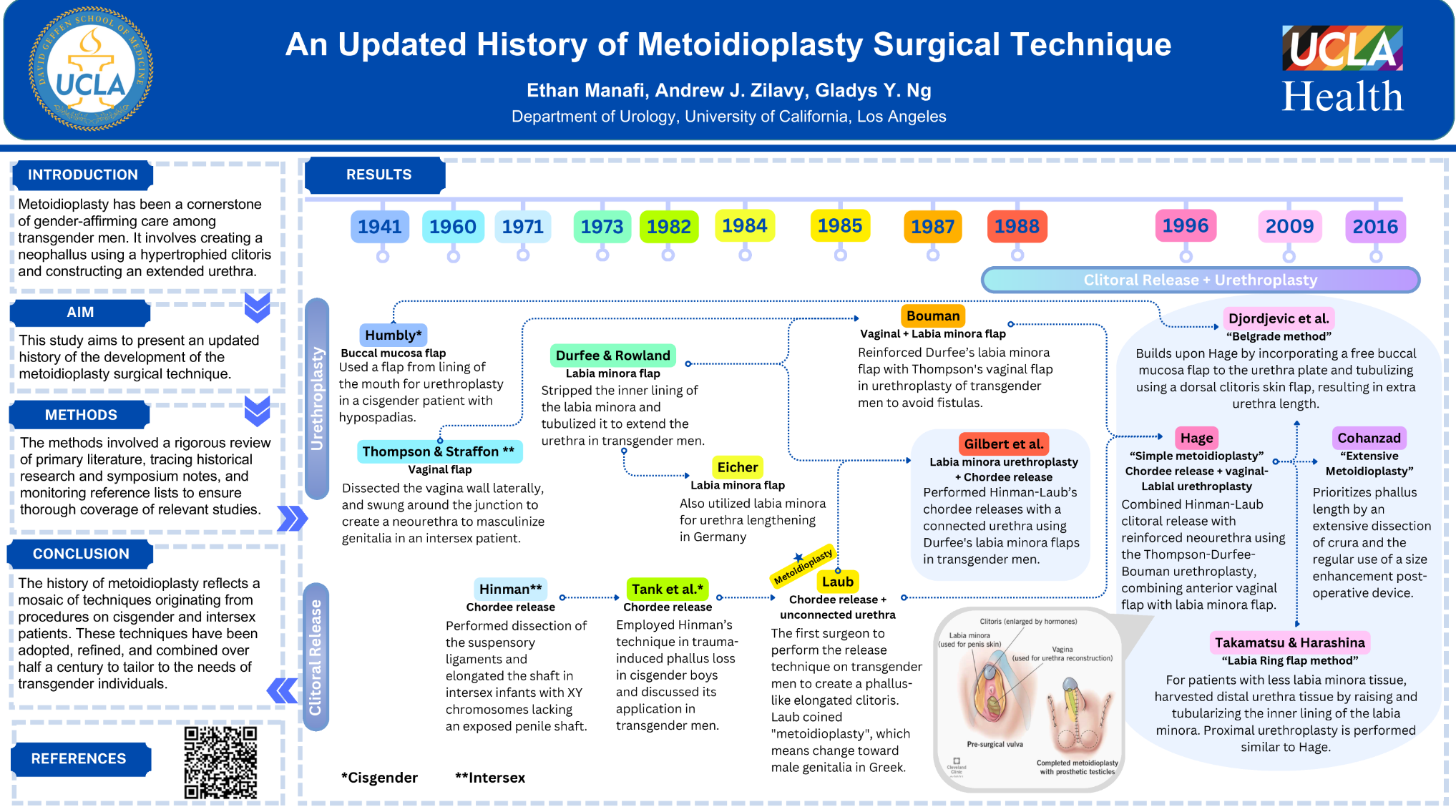
A Visual History of Metoidioplasty: Techniques and Milestones
“An Updated History of Metoidioplasty Surgery Technique” is a visual timeline created by researchers at UCLA in 2024 that traces the evolution of Metoidioplasty based on academic studies and symposium records. It also highlights relevant techniques originally developed for cisgender and intersex patients. The timeline ends in 2016, so it does not include more recent innovations such as Extended Metoidioplasty, TCM, or the ZSI erectile implant. As expected, it also omits Genitalplasty and Centurion Metoidioplasty, neither of which has been formally documented in peer-reviewed literature.
References
- Lebovic GS, Laub DR. Metoidioplasty. In: Ehrlich RM, Alter GJ, editors. Reconstructive and Plastic Surgery of the External Genitalia. Philadelphia: WB Saunders Co.; 1999. p. 355–60.
- Hage JJ. Metoidioplasty: an alternative phalloplasty technique in transsexuals. Br J Plast Surg. 1996;49(3):199–204.
- Takamatsu A, Ishii T, Fukunaga M, et al. A new urethroplasty for metoidioplasty in female-to-male transsexuals. Int J Urol. 2003;10(7):383–6.
- Djordjevic ML, Stanojevic D, Bizic M, Kojovic V, Majstorovic M, Vujovic S, Milosevic A, Korac G, Perovic SV. Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience. J Sex Med. 2009 May;6(5):1306-13. doi: 10.1111/j.1743-6109.2008.01065.x. Epub 2009 Oct 27. PMID: 19175859.
- Takamatsu A, Harashina T. Labial ring flap: a new flap for metaidoioplasty in female-to-male transsexuals. J Plast Reconstr Aesthet Surg. 2009 Mar;62(3):318-25. doi: 10.1016/j.bjps.2008.11.038. Epub 2009 Jan 24. PMID: 19168410.
- Cohanzad S. Extensive
metoidioplasty as a technique capable of
creating a compatible analogue to a
natural penis in female transsexuals.
Aesthetic Plast Surg.
2016;40(1):130–8.
doi:10.1007/s00266-015-0607-4. PMID:
26744289.
- Cohanzad S. Penile Improvement Protocol in postoperative management of patients undergoing metoidioplasty. Aesthetic Plast Surg. 2016;40(6):947–53. doi:10.1007/s00266-016-0700-3. PMID: 27646118.
- Djordjevic ML, Bizic M, Stanojevic D, et al. Metoidioplasty: techniques and outcomes. Transl Androl Urol. 2019. doi:10.21037/tau.2019.06.12.
- Morrison, S. D., Morris, M. P., Mokken, S. E., Buncamper, M., & Özer, M. (2022). Technical refinements to extended metoidioplasty without urethral lengthening: Surgical technique. Plastic and Reconstructive Surgery – Global Open, 10(2), e4101. doi.org/10.1097/GOX.0000000000004101
- Barroso U Jr, Venturini B, Massuqueto E, Prado F, Castro A, Santos H. Total corpora mobilization for penile reconstruction. Int Braz J Urol. 2022;48(5):878–9. doi:10.1590/S1677-5538.IBJU.2022.0177. PMID: 35838516; PMCID: PMC9388176.
- Monchablon B, Morel-Journel N, Carnicelli D, Jurek L, Ruffion A, Neuville P. Surgical outcomes, motivations, sexuality, and urinary function of metoidioplasty with semi-rigid prosthesis. Int J Transgend Health. 2023;26(1):63–72. doi:10.1080/26895269.2023.2279273.
- Stojanovic B, Djordjevic ML. Updates on metoidioplasty. Neurourol Urodyn. 2023;42(5):956–62. doi:10.1002/nau.25102.
- Cohanzad S. Eight-year follow-up on postoperative improvement protocol in extensive metoidioplasty transgenders: A case series. Chin J Plast Reconstr Surg. 2023;5(3):115–9. doi:10.1016/j.cjprs.2023.08.003.
Last updated: 05/29/25