Metoidioplasty.net » Metoidioplasty Procedures
Centurion Metoidioplasty
Centurion Metoidioplasty is a masculinizing genital surgery developed by Dr. Peter Raphael in Texas, USA, and first performed in 2002. While often grouped with Full Metoidioplasty techniques like the Belgrade method, Centurion includes a key refinement: the use of the round ligaments to enhance girth and support of the neophallus. This procedure provides a natural-looking, small penis with preserved sensation and erectile function, using only native genital tissue.
Although it was likely developed independently, Centurion shares the core components of Full Metoidioplasty, including urethral lengthening to enable standing urination and scrotoplasty with testicular implants.
How It Works
During the procedure, the clitoris is released by dividing the suspensory ligaments to maximize visible length. The urethra is extended to the tip of the neophallus using local skin flaps, which are joined around a catheter to form the tube. This allows for urination while standing.
The round ligaments, which run along the labia, are mobilized and rotated medially to wrap along the shaft of the neophallus, increasing girth and structural support. This not only enhances appearance but also reduces the risk of postoperative retraction, particularly in patients with a larger mons pubis.
After vaginectomy is performed*, a scrotum is created by fusing the labia majora, leaving a central sac for testicular implants, which are placed during the same surgery.
Operating time is approximately 3 hours without hysterectomy and 4 hours if a hysterectomy is also performed during the same session.
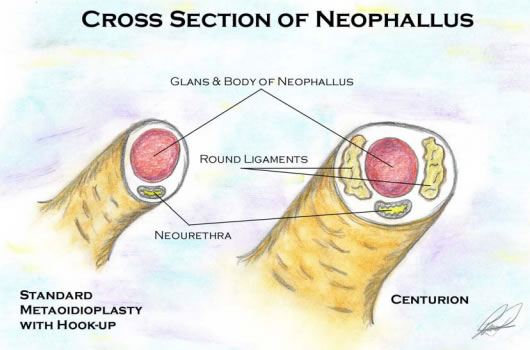
Illustration from "Female-to-Male Urogenital Reconstruction: The Centurion Procedure"
*Important Note on Dr. Peter Raphael’s Approach to Vaginectomy
Dr. Raphael uses a unique method for vaginectomy that differs from traditional techniques. Instead of removing the vaginal lining through dissection or ablation, his approach closes the vaginal canal internally at the top and bottom without removing the tissue itself.
In this technique, the upper end of the vaginal canal is sealed from inside the abdomen, and then the natural vaginal opening is closed (perineoplasty). This effectively turns the vaginal canal into a closed space. It avoids operating near structures like the bladder, bowel, or rectum—areas where complications, while rare, can sometimes occur. Any secretions from the residual vaginal tissue are safely reabsorbed by the body.
This approach is quite different from traditional colpectomy (removal of the vaginal lining) and colpocleisis (closure of the vaginal canal). Patients considering vaginectomy should consult with experienced surgeons to understand which method best aligns with their anatomy, goals, and surgical plan.
Expected Results
Centurion typically results in a natural-appearing penis with preserved erogenous sensation and the ability to achieve spontaneous erection. However, the resulting phallus is usually too small for penetrative sex, with average lengths similar to other metoidioplasty outcomes (often between 4 and 7 cm, depending on anatomy and hormone response).
Patients are generally able to urinate while standing, and the appearance of the scrotum is realistic, with a single fused sac and two testicular implants. Because the procedure uses native genital tissue only, there are no visible donor site scars, which may be a significant benefit for many patients.
Risks and Complications
While Centurion Metoidioplasty is generally safe when performed by an experienced surgeon, complications may occur, including:
- Urethral fistula (an abnormal connection between the urethra and skin)
- Urethral stricture (narrowing of the urethra, potentially affecting urine flow)
- Scrotal implant extrusion (rejection or displacement of testicular implants)
Some patients may require revisions to improve appearance or address minor functional issues.
Recovery
A Foley catheter remains in place for approximately 2 weeks after surgery to allow the new urethra to heal. (Although not mentioned in the original documentation, current best practices also include a suprapubic catheter to divert urine during urethral healing.) Most patients return to normal, non-strenuous activity within 2 to 4 weeks, though full healing can take longer. Revision procedures may be performed later if needed, but many patients complete their transition with this single operation.
Who Is This Procedure Right For?
Centurion Metoidioplasty is suited to patients seeking a natural-looking phallus that is girthier than the typical Metoidioplasty, standing urination, and preserved sexual sensation. However, it’s not the ideal choice for patients who prioritize phallus size sufficient for penetration, or those with higher BMI or significant mons pubis fat, as excess adipose tissue can obscure length and affect urinary function.
Eligibility
To be eligible for Centurion, patients generally must meet the following criteria:
- 1–2 years on testosterone, with adequate growth of the clitoris
- Diagnosed with persistent gender dysphoria
- Capacity to consent and make informed decisions
- Stable mental health
Surgeons
While Dr. Peter Raphael in Plano, Texas is the only surgeon publicly known to offer the Centurion procedure, it is possible that other surgeons have independently incorporated the use of round ligaments into their own variations of Full Metoidioplasty.
Relevant Journal Articles
There are no peer-reviewed publications on the Centurion technique, but it shares foundational principles with Full Metoidioplasty methods such as the Belgrade procedure. The only known published information about the Centurion can be found in the PDF, Female-to-Male Urogenital Reconstruction: "The Centurion Procedure" By Tex McFaden, DO.
Last updated: 05/29/25